By Denis G. Rancourt, PhD
Citation: Rancourt, DG. Opinion: Invalidity of counterfactual models of mortality averted by childhood vaccination. CORRELATION Research in the Public Interest, Report, 29 January 2025. https://correlation-canada.org/opinion-childhood-vaccination-mortality-averted
DOI: https://doi.org/10.31219/osf.io/amfxw_v1
I express and support the opinion that all models that purport to calculate the mortality (infant mortality in particular) averted by vaccine programmes are invalid because they are based on inputs of vaccine efficacy and pathogen prevalence and virulence that are themselves invalid. Even with ideal testing, the counterfactual number of deaths from a presumed pathogen if the targeting vaccination programme was not implemented is impossible to calculate reliably because it is contrary to biological reality: the deaths of concern are always complex non-linear events that involve several interacting contributing factors that do not have additive effects. Furthermore, infant mortality factors other than vaccination are highly variable and overwhelmingly more important than any presumed vaccine benefit; predominantly, deleterious effects of nutritional deficiencies and of relentless exposures to challenges from toxic living environments. The underlying cause is so-called failed-state extreme poverty due to structural financial exploitation that is not being addressed. There is no known example of a drop in measured infant or child mortality temporally associated with the rollout of a childhood vaccination programme. Independent studies suggest that, contrary to dogma, excess infant mortality (not averted infant mortality) is associated with vaccine programme rollouts and maintenance. Using yearly infant all-cause mortality rate directly, I estimate approximately 100 million vaccine-rollout-associated infant deaths 1974-2024 worldwide, with the caveat of concomitant largescale economic transformations. I conclude, overall, that the longstanding industry of infant vaccination programmes is a baseless fraudulent enterprise of exploitation.
Researchers and I at CORRELATION and collaborators continue to be engaged in a broad research program of all-cause mortality and its associations with various factors: https://correlation-canada.org/research/
1 Current epidemiological modelling context 3
2 Crux and purpose of this paper 8
3 Illustrative example of the 2024 study of Shattock et al. published in Lancet 10
4 Invalidity of the inputs for counterfactual models of mortality averted by vaccination.. 16
4.2 There are no adequate and policy-grade clinical trials for infant vaccine safety. 18
There are no direct field demonstrations that global infant vaccination programmes reduce infant or childhood mortality, in low-, middle- or high-income countries or communities. The World Health Organization (WHO) gratuitously claims that millions of lives are saved every year (WHO, 2019) but early skepticism (England, 1978; Hendrickse, 1975) and contrary evidence persist (Ahmed et al., 2000; Cutler et al., 2006; and Section 5, below).
In recent years tentative and untethered models of epidemiological forecasting and epidemiological counterfactual analyses producing unlikely results have flooded the medical literature, including in leading journals.
These models incorrectly and uncritically rely entirely on estimates of vaccine efficacy and not on any field observations whatsoever of actual deaths and their specific individual-level circumstances.
The said flood of these kinds of models is cause for legitimate concern regarding public health policy guidance. In the words of Ioannidis et al. (2022):
“Epidemic forecasting has a dubious track-record, and its failures became more prominent with COVID-19. Poor data input, wrong modeling assumptions, high sensitivity of estimates, lack of incorporation of epidemiological features, poor past evidence on effects of available interventions, lack of transparency, errors, lack of determinacy, consideration of only one or a few dimensions of the problem at hand, lack of expertise in crucial disciplines, groupthink and bandwagon effects, and selective reporting are some of the causes of these failures. …” (Abstract, p. 423)
“… Poorly performing models and models that perform well for only one dimension of impact can cause harm. It is not just an issue of academic debate, it is an issue of potentially devastating, wrong decisions (ref).” (p. 432)
In counterfactual analysis “the outcomes of the intervention are compared with the outcomes that would have been achieved if the intervention had not been implemented.” (BGI Consulting, 2007)
The present lack of standards in forecasting and counterfactual exercises gives more than a little credence to the words of former Lancet editor Richard Horton (2004):
“… medical journals have become an important but underrecognized obstacle to scientific truth-telling. Journals have devolved into information-laundering operations for the pharmaceutical industry.”
And more than a little credence to the thesis of former BMJ editor Richard Smith (2005):
“Medical journals are an extension of the marketing arm of pharmaceutical companies.”
The publishing surge of at best questionable forecasting and counterfactual models of mortality averted by vaccination campaigns and programmes is not unrelated to the tsunami of systematic reviews and meta-analyses used in-effect to cover up wholly inadequate and outright concocted clinical trials of vaccine efficacy (Gøtzsche, 2013; Ioannidis, 2016a, 2016b), on which the models are based.
A few examples of demonstrably false models in the COVID-19 context are as follows.
Rancourt et al. (2022) showed that a counterfactual analysis published by Canadian government scientists, concluding that approximately 1 million lives had been saved by government COVID-19 measures in Canada, including vaccination, is untenable.
Rancourt and Hickey (2023) showed that the counterfactual analysis of Watson et al. (2022), published in The Lancet Infectious Diseases and concluding that some 14 to 20 million worldwide deaths were prevented by COVID-19 vaccinations, is impossible.
Separately, and contrary to the Watson et al. (2022) counterfactual, Rancourt et al. (2023, 2024) showed that COVID-19 vaccination rollouts are systematically and strongly associated in time with surges and peaks in excess all-cause mortality, quantified to approximately 17 million vaccine-rollout-associated excess deaths worldwide during the declared pandemic. Also, see the discussion of this number of vaccine-rollout-associated deaths by Rancourt (2024).
Ioannidis, with co-authors (2024), incorrectly projected that 1.4 to 4.0 million lives were saved by COVID-19 vaccinations worldwide, until October 2024. The underlying assumptions in their calculation are unjustified. Their estimate is a counterfactual comparison but not one that uses epidemiological modelling of contagious spread to estimate the deaths without intervention. Instead, they use seroprevalence data and reported COVID-19 deaths. Nonetheless, their analysis illustrates the core difficulties with all epidemiological counterfactual and forecast models based on presumed vaccine efficacy and estimated mortality if vaccination had not been implemented.
The said core difficulties are this. One must derive the number of deaths, D0, that should occur from the presumed pathogen in the absence of the intervention (i.e., without vaccination) and use an estimate of the vaccine efficacy, Ev, in preventing deaths. Ev is the vaccine-attributed reduction of probability of death per person presumed to be fatally infected. In simple terms, the number of lives saved, Ls, (or deaths averted) is then the product of D0, Ev and vaccine coverage Cv:
Ls = D0 x Ev x Cv. (1)
Cv can be known with relative certainty, whereas D0 and Ev are disjunctively and irreparably problematic. Ioannidis et al. (2024) do not resolve or sufficiently recognize these problems:
Antibody tests (seroprevalence) approved for presumed COVID-19 and used in high-profile epidemiological studies can be shown to be invalid (Rancourt, 2021).
Regarding the likelihood that published clinical trial findings of COVID-19 vaccine efficacy are valid, the landmark report of Gøtzsche (2013) leaves little doubt that such trials for any vaccine cannot be trusted whatsoever, given the structural nature of the industry, not to mention the exceptionally politicized and captured institutional context of the declared COVID-19 pandemic. And we should be cognizant of the following partial generic list provided by Smith (2005):
Examples of Methods for Pharmaceutical Companies to Get the Results They Want from Clinical Trials
Furthermore, Ioannidis et al. (2024) perform their projection of lives saved without tethering their estimate to measured all-cause mortality (by time, by jurisdiction, and by age group). They simply neglect to examine any connection to hard mortality data and they state, under the heading “General principles”, in their Appendix 1:
“In calculating our estimates, we do not consider deaths and other consequences from adverse effects of SARS-CoV-2 vaccines, nor do we make any adjustment for the quality of life-years saved. Moreover, we do not attempt to calculate indirect effects of COVID-19 vaccination which may have modulated excess deaths through an impact on non-COVID-19 causes of death.”
It is a common characteristic of counterfactual and forecasting models reporting on benefits of interventions not to attempt to tether their often fantastic results to hard all-cause mortality data (e.g., Rancourt and Hickey, 2023).
There are many more failures of epidemiological modelling of the declared COVID-19 pandemic than the few mentioned above (Ioannidis et al., 2022). As though buoyed by this COVID-19 flood of epidemiological modelling, and possibly motivated by rising Covid-era vaccine hesitancy of parents in the Western world (Lazarus et al., 2023), many published articles are now making fantastic claims about worldwide benefits from childhood vaccination programmes, which are the main subject of the present paper.
Recently, many modelling studies have been published in both specialized and leading medical journals, in which the authors purport to reliably estimate historic mortality averted by global vaccination programmes, especially childhood vaccination programmes. An incomplete list of these journal articles includes: Auzenbergs et al., 2023; Carter et al., 2024; Cutts et al., 2020; Echeverria-Londono et al., 2021; Gaythorpe et al., 2021; Li et al., 2021; Mesa et al., 2023; Rouch et al., 2007; Shattock et al., 2024; Toor et al., 2021; Verguet et al., 2015; Winter et al., 2022; and references therein.
In the present paper, following Section 1, I argue that all such models of mortality averted by universal (often childhood) vaccination programmes are invalid because of two fatal disjunctive difficulties. The said fatal disjunctive difficulties are:
I argue that the proverbial computing term “garbage in, garbage out” pre-eminently applies in these circumstances.
The published modelling studies fail to follow scientific norms by never including propagated error bounds starting from realistic assessments of the core uncertainties. If they did, they would not have any results to report beyond inadequacy of the approach.
The utilized guesstimates of deaths caused by the specific presumed pathogen that would have occurred if the childhood vaccinations had not been implemented (D0, Equation 1) most often rely on siloed epidemiological models of spreading contagion (so-called dynamic models), which are not validated, and which themselves are fundamentally not reliable. The said guesstimates are not anchored in comparative comprehensive field-based studies, which are virtually never undertaken.
If the researchers duly attempted to validate or justify their estimates of averted mortality by comparisons with the historic evolution of all-cause or cause-specific and all-ages or age-specific mortality, they would encounter the insurmountable difficulty that early-life mortality rates are predominantly determined by many interacting factors other than vaccination, and that any vaccination contribution cannot independently be ascertained from the available data (Sections 4.3 and 4.4).
Finally, there is the inconvenient fact that, to my knowledge and until proven otherwise, there is no known example of a drop in measured infant or child mortality temporally associated with any rollout of a childhood vaccination campaign or initiation of a permanent childhood vaccination programme. On the contrary, comparative studies report a positive association between childhood mortality and childhood vaccination doses administered (Section 5).
A recent example of the type of study that concerns us is the study by Shattock et al. (2024).
The claims of Shattock et al. (2024) are not modest, with outcomes cited to 3 significant figures (Stewart, 2024):
“Findings ― Since 1974, vaccination has averted 154 million deaths, including 146 million among children younger than 5 years of whom 101 million were infants younger than 1 year. For every death averted, 66 years of full health were gained on average, translating to 10·2 billion years of full health gained. We estimate that vaccination has accounted for 40% of the observed decline in global infant mortality, 52% in the African region. In 2024, a child younger than 10 years is 40% more likely to survive to their next birthday relative to a hypothetical scenario of no historical vaccination. Increased survival probability is observed even well into late adulthood.”
The claimed worldwide 154 million deaths averted by vaccination intervention in the 50 years (1974-2024) corresponds to 5.7 % of worldwide deaths, on a per year basis, which is a fantastic claimed medical achievement. Some might reasonably call it unbelievable.
The Shattock et al. (2024) claim is aligned with a media statement made by the WHO for 2019 (WHO, 2019):
“Vaccine hesitancy – the reluctance or refusal to vaccinate despite the availability of vaccines – threatens to reverse progress made in tackling vaccine-preventable diseases. Vaccination is one of the most cost-effective ways of avoiding disease – it currently prevents 2-3 million deaths a year, and a further 1.5 million could be avoided if global coverage of vaccinations improved.”
The 2-3 million averted deaths a year claimed by the WHO corresponds to 100-150 million averted deaths in the 50-year period studied by Shattock et al. (2024), and the further 1.5 million averted deaths a year from complete vaccine coverage would correspond to an approximately 20% global reduction in infant mortality, in the absence of any other intervention, a truly remarkable feat if it was realistic.
The Shattock et al. (2024) “study was funded by WHO. … Model outputs were provided by the Vaccine Impact Modelling Consortium (VIMC...) … VIMC is funded by Gavi, the Vaccine Alliance and the Bill & Melinda Gates Foundation.” (p. 2315)
The Declaration of interests of the authors is given as (p. 2315):
“CLT and KAMG assert that their employer, Imperial College, receives funding for the Vaccine Impact Modelling Consortium from the Bill & Melinda Gates Foundation; Gavi, the Vaccine Alliance; and the Wellcome Trust. CLT has received consulting fees from GSK for attending an advisory board meeting on CMV vaccines in May, 2022 and is pro bono Chair of the Scientific Advisory Panel of the Meningitis Research Foundation. HF asserts that her employer, London School of Hygiene & Tropical Medicine, receives funding for the Vaccine Impact Modelling Consortium from the Gates Foundation. JFM asserts that his employer, University of Washington, receives grant funding from Gavi and from the Gates Foundation. KB and KMT assert that their organisation Kid Risk holds a cooperative agreement with the US Centers for Disease Control and Prevention and holds grants from the Gates Foundation. MJF asserts that his employer, Penn State University, is a subrecipient of funds from Imperial College London for a grant from Gavi and that he holds grants from the Gates Foundation and the US National Science Foundation. MJ asserts that his employer, London School of Hygiene & Tropical Medicine, receives funding from the UK National Institute of Health Research, RCUK; the Gates Foundation; Gavi; the Wellcome Trust; WHO; the European Commission; the US Centers for Disease Control and Prevention; the Hong Kong Special Administrative Region Government; and the Task Force for Global Health. RAH and SPS assert that their employer, University of Cape Town, receives grant funding from the African Field Epidemiology Network and the US Centers for Disease Control and Prevention. RGW asserts that he receives funding from the Wellcome Trust (grant numbers 218261/Z/19/Z), National Institutes of Health (1R01AI147321-01, G-202303-69963, and R-202309-71190), European and Developing Countries Clinical Trials Partnership (RIA208D-2505B), UK Medical Research Council (CCF17-7779 via SET Bloomsbury), UK Economic and Social Research Council (ES/P008011/1), Bill & Melinda Gates Foundation (INV-004737 and INV-035506), and WHO (2020/985800-0). AL, KLO-B, NB-Z, PL, RCWH, and SYS work for WHO. All other authors declare no competing interests.”
Such ties are common in these kinds of articles in leading journals, not to mention the interests of the journals, editors and reviewers (Gøtzsche, 2013).
I next examine the stated methods used by Shattock et al. (2024). Going beyond the broad non-specific statements such as “We developed a standardised analytical framework to estimate vaccine impact per fully vaccinated person over time, synthesising the results of 22 models and applying regression-based imputation methods to ensure geographical and temporal completeness.” (p. 2308), it is clear that Shattock et al. (2024) applied the usual approach (Equation 1: Ls = D0 x Ev x Cv): “Vaccine efficacy and vaccine coverage were combined to produce an estimate of effective vaccine coverage, which was then used to estimate disease-attributable mortality and morbidity in a hypothetical scenario of no historical vaccination for the nine vaccines considered (appendix pp 25–26).” (p. 2310)
Shattock et al. (2024) used two different methods to estimate counterfactual deaths, D0, depending on whether the presumed pathogen was considered to be either contagious or of a background-prevalence nature. For contagious pathogens, they used so-called “published dynamic models”, whereas for the background-prevalence pathogens they used published prevalence determinations (p. 2310).
The so-called dynamic models are standard epidemiological models of contagious spread, infused with the theoretical impacts of concomitant vaccine administration. This allowed Shattock et al. (2024) to theoretically account for so-called immune waning (part of vaccine efficacy, estimated from clinical trials) and to theoretically include the effects of boosting or of not fully vaccinated individuals.
The so-called dynamic models themselves have not been validated and have insurmountable difficulties related to high sensitivity to transmission, recovery and virulence input parameters, if their fundamental underlying assumptions are even valid (e.g., Hickey and Rancourt, 2023a, 2023b). For example, in particular, the needed infectious contact frequencies are essentially impossible to empirically determine (e.g., Hickey and Rancourt, 2023a, 2023b). Also, such models are in their infancy regarding realistic geo‑temporal spread of infections (Keeling and Rohani, 2008).
Therefore, the study of Shattock et al. (2024) collapses on examination of its premises regarding D0 and Ev, defined in Equation 1.
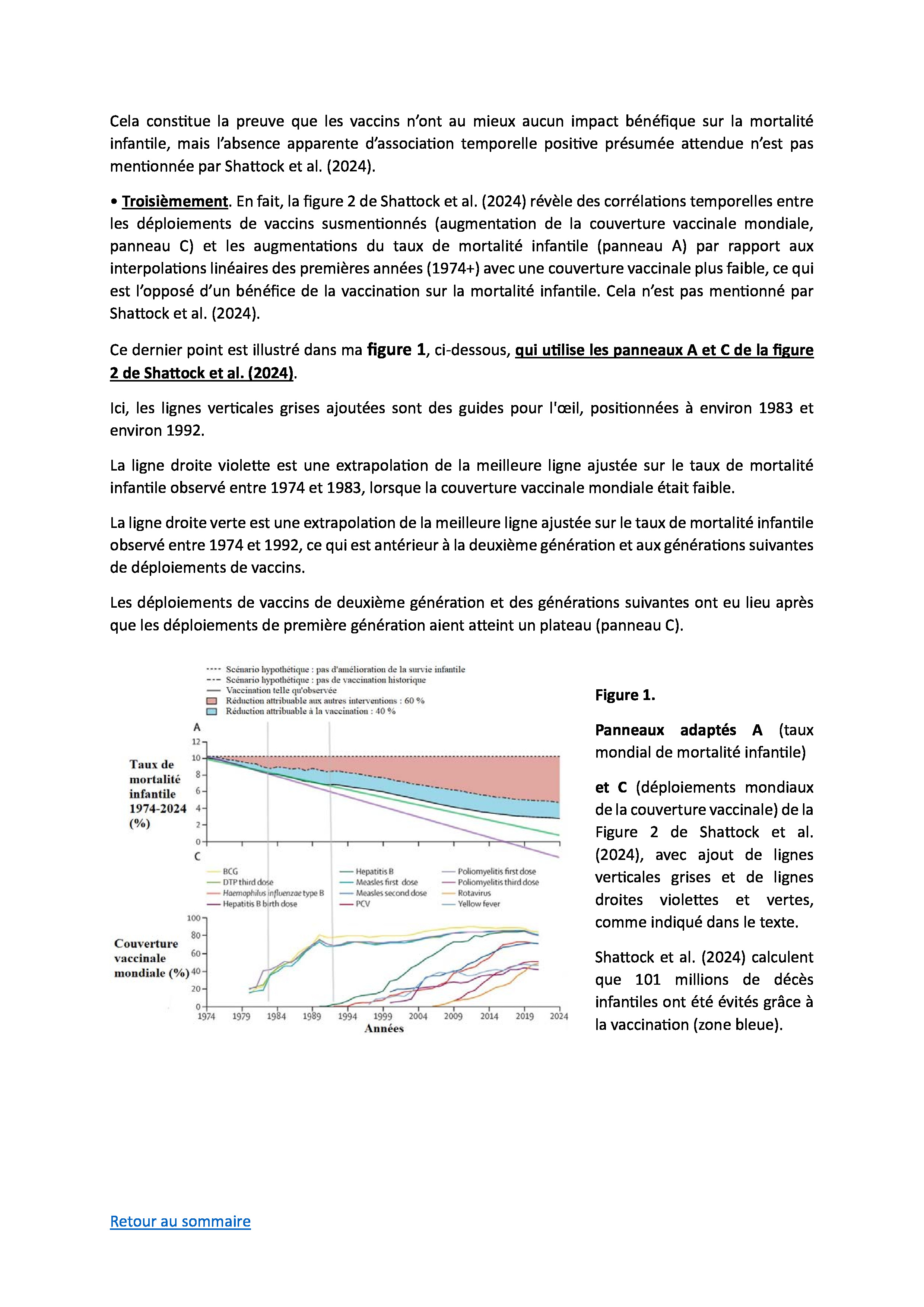
Shattock et al. (2024) go further. For their Figure 2, they plot a hypothetical constant no‑improvement global infant mortality scenario (1974-2024) arbitrarily fixed at the 1974 value, a hypothetical no‑vaccination scenario, and the as-observed actual infant mortality (with vaccination), all as functions of time since 1974. The constructed graph corresponds to vaccination being responsible for 40 % of the reduction in infant mortality since 1974, and 25 % in 2024. These, again, are fantastic claims of life-saving benefits from the medical interventions as sole factors.
Beyond the fantastic magnitude of the claimed effect, Shattock et al. (2024)’s Figure 2 is incorrectly presented and interpreted regarding three other aspects:
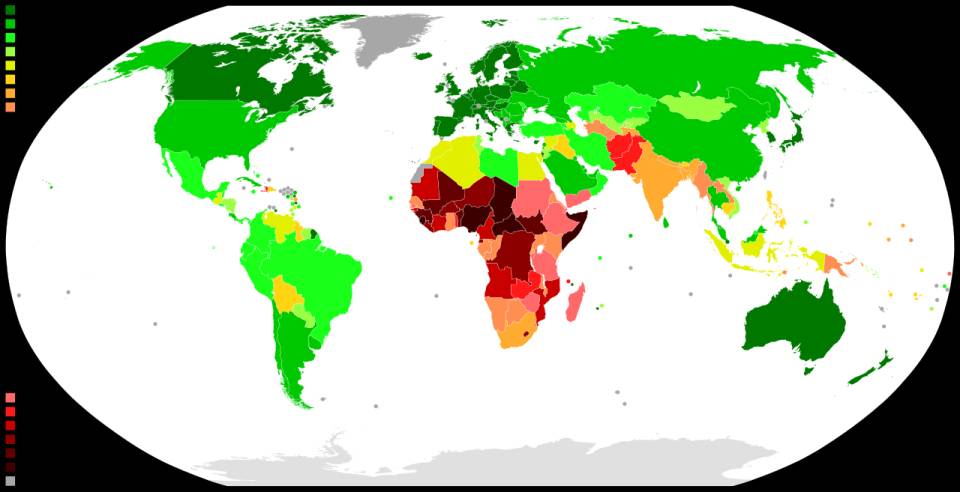
The latter point is illustrated in my Figure 1, below, which uses panels A and C from Shattock et al. (2024)’s Figure 2. Here, the added grey vertical lines are guides to the eye, positioned at approximately 1983 and approximately 1992. The purple straight line is an extrapolation from the best adjusted line on the as-observed infant mortality rate between 1974 and 1983, when little global vaccine coverage was occurring. The green straight line is an extrapolation from the best adjusted line on the as-observed infant mortality rate between 1974 and 1992, which is prior to the second and later generations of vaccine rollouts. The second and later generations of vaccine rollouts occurred after the first-generation rollouts had plateaued (panel C).
Figure 1. Adapted panels A (global infant mortality rate) and C (global vaccine coverage rollouts) from Shattock et al. (2024)’s Figure 2, with added grey vertical lines, and added purple and green straight lines, as discussed in the text. Shattock et al. (2024) calculate that 101 million infant deaths were averted by vaccination (blue area).
Shattock et al. (2024) calculate ― remarkably using 3 significant numbers and no confidence interval ― that 101 million deaths of infants younger than 1 year were averted by vaccination (p. 2312), which is the blue area in their Figure 2 (my Figure 1). In fact, if anything, the opposite may be true. The difference between my purple-line extrapolation (which assumes a constant rate of reduction of infant mortality rate from improvements of factors other than vaccination, needing to be corrected to give a positive rate after approximately 2016) and the as-observed infant mortality rate (solid black line, panel A) corresponds to approximately 100 million vaccine-rollout-associated infant deaths 1974-2024 worldwide. If large concomitant deleterious socio-economic changes did not occur (starting in the 1980s and in the 1990s), this would imply that approximately 100 million infant deaths (worldwide, 1974-2024) would not have occurred if the intervention of vaccinations had not been implemented. Shattock et al. (2024) did not consider this, whereas it is apparent in their own data.
Here, I elaborate each of the sources mentioned above of fundamental invalidity of the usual forecasting and counterfactual models of mortality averted by vaccination.
The published clinical trials of vaccine efficacy cannot be taken to be valid because the entire clinical trial and publication process is overwhelmingly controlled by an industry making large profits from the vaccines, and this industry has amply, historically, consistently and repeatedly demonstrated its willingness to act fraudulently at the expense of endangering the public (Gøtzsche, 2013). Gøtzsche (2013)’s landmark documented overview proves that the degree of deceit and corruption is astronomical and deeply entrenched. Reasonable researchers must conclude that clinical trial evaluations of vaccine efficacy are unusable. See also the career-informed corroborating assessments of editors at leading medical journals: Lancet, Horton (2004); and BMJ, Smith (2005).
Even relying solely on the tunnelled and sanitized published scientific-journal reports ― without any inside knowledge or access to the industry-locked patient-level trial data ― many academic researchers had in 2003 already demonstrated a strong (4-fold) funding bias in published results (reviews: Bekelman et al., 2003; Lexchin et al., 2003). See also: Elisha et al. (2021).
Irrespective of the overwhelming evidence of corruption in the conduct of clinical trials, Krauss (2018) explained that defining features of randomized clinical trial design make them intrinsically unreliable in most applications, in his article entitled “Why all randomised controlled trials produce biased results” (Krauss, 2018). Major problems identified by Krauss are many and include these structural features:
Regarding lack of transparency, in the words of Mangin et al. (2018), in the Western-nation geriatric context, their 6th recommendation is:
“6. Acknowledge and address commercial influences on polypharmacy: trial results should not be implemented in older adults unless access to all available patient-level data is provided. Appropriate outcome measures should be required before licensing indications that include older populations.
The degree to which commercial interests can potentially distort scientific data is well documented [126,127,128,129,130,131]. Trials can be structured to provide commercially favorable results and there is limited access to patient-level trial and adverse-event data, which are grounds for precautionary prescribing [132]. Use of intermediate outcomes, publication bias, and overhyping of new or immature research results by media and pharmaceutical companies result in a research narrative that overestimates efficacy, underestimates harms, and fuels IMUP [inappropriate medication use and polypharmacy] [133,134,135]. Evidence bias is commonly compounded by biased interpretation, where key opinion leaders have industry conflicts of interest [136].”
Access to all patient-level data (not just “available” patient-level data, including patients that were excluded in the in-trial process) is essentially never granted to independent or competing researchers by the controlling pharmaceutical corporation, in any clinical trial, and can be presumed to be in-effect hidden from even the government agencies. Therefore, following the above-noted principle expressed by Mangin et al. (2018), “trial results should not be implemented”. I don’t see any good reason why this principle would not be universally applied in all circumstances in which a clinical trial is needed to tease out any benefit from the promoted medical intervention, or in which a small number of dropped or different patients could make the claimed benefit disappear.
Regarding infants, unhealthy infants are not enrolled in a clinical trial, whereas, in practice, unhealthy infants are vaccinated. That unhealthy infants are routinely vaccinated is especially true in the low-income countries with (United Nations) UN‑promoted universal vaccination programmes, whereas the clinical trials were virtually always performed on healthy children in Western facilities. Furthermore, clinical trial enrolment exclusion criteria are strictly imposed (and are not applied transparently), whereas the in-field decision not to vaccinate because of poor health is more fluid and left to individual clinical or practitioner judgement.
Infants and children are distinct from adults, especially in regards to their developing gut microbiomes and immune systems, and especially in the first several months and up to 3 or more years of age (Arrieta et al., 2014; Laforest-Lapointe and Arrieta, 2017; Olin et al., 2018; Ygberg and Nilsson, 2012).
Therefore, any clinical trial intended to establish safety of a childhood vaccine administered to an infant must monitor participant health at least up to 3 or more years in age. This is never done (Brand and Siri, 2024; ICAN, 2017).
Any clinical trial intended to establish safety of a childhood vaccine administered to an infant must include a control arm with either no vaccination or an inert placebo. This is virtually never done (Brand and Siri, 2024; ICAN, 2017). There is no valid reason not to have a control arm or to insist on using an active placebo, because evaluating clinicians, statisticians, caregivers and parents can be blinded to the intervention, and the infants and children are not subjectively self-reporting the adverse-effect outcomes. Without such a control arm (no vaccination or inert placebo), safety is not evaluated.
Most importantly, any clinical trial intended to establish safety of a childhood vaccine administered to an infant must use participants having health statuses and vulnerabilities representative of the actual in-field target population for the vaccine. This is never done because it is strictly unethical to expose a vulnerable or fragile infant to a non-benign and untested preventative medical intervention.
Yet, on a population scale, with actual vaccination programmes, many subjects will not be excluded who have poor health status and significant vulnerabilities. This is especially true in low-income countries and communities where malnutrition and its devastating health consequences are the norm (Ahmad et al., 2000; Bailey et al., 2015; England, 1978; Gombart et al., 2020; Hendrickse, 1975; Katoch, 2022; Katona and Katona-Apte, 2008; Keusch, 2003; Rodiguez et al., 2011; Scrimshaw, 2003; Scrimshaw et al., 1968).
Therefore, so-called randomized clinical trials of vaccines for infants provide no information about safety, and do not allow one to estimate impacts on infant mortality from vaccine adverse effects and toxicity, especially in low-income countries. Vaccine safety cannot be assumed in forecasting and counterfactual theoretical models of mortality. Published clinical trial results claiming vaccine efficacy (Section 4.1) do not demonstrate vaccine safety for real-world applications.
Even if valid vaccine safety clinical trials on infants and children existed from Western-world clinics and hospitals, which they do not (Brand and Siri, 2024; ICAN, 2017), the trial subjects would not be comparable to the malnourished and differently challenged infants and children in low-income countries. Again, there is a strong gut microbiome to immune system interaction in the immune development of infants and children, which determines survival and health (Arrieta et al., 2014; Laforest-Lapointe and Arrieta, 2017; Olin et al., 2018; Ygberg and Nilsson, 2012). For example, gut microbiome adaptation even compensates for the challenges of undernourishment, and this alone is good reason not to artificially interfere directly with immunity.
A rare example involving candidate clinical trials regarding harm in vaccinating vulnerable infants is the case of clinical trials for cardiorespiratory events in preterm infants, which were already known to occur from retrospective and observational studies. There are two randomized comparative clinical trials (2-month vaccination versus no vaccination) for a defined outcome observed within 48 hours (Carbone et al., 2008; Greenberg et al., 2025). Both had small clinically selected cohorts (approximately 100 in each comparison group, selected by health status prior to randomization) and insufficiently small numbers of observed events (approximately 10). Both trials carefully avoided infant participants with negative or unstable health conditions. The two trials report contrary conclusions. The trial finding no harm from vaccination ambiguously states “Infants who required assisted ventilation or tracheostomy during the study were excluded from participation.” (p. e1086, Carbone et al., 2008), and does not report the funding sources of its organization. The other trial has the following funding and interests statements (Greenberg et al., 2025) (p. E8):
Funding/Support: This study was supported by the US Centers for Disease Control and Prevention (Clinical Immunization Safety Assessment Project contracts …).
Role of the Funder/Sponsor: The US Centers for Disease Control and Prevention participated in the design and conduct of the study; interpretation of the data; preparation, review, and approval of the manuscript; and the decision to submit the manuscript for publication. …
Conflict of Interest Disclosures: Dr Greenberg reported consulting for Oak Hill Bio outside the submitted work. Dr Staat reported grants from Pfizer (respiratory syncytial virus vaccine study), Merck (rotavirus study), and Cepheid (respiratory infection diagnostics) outside the submitted work. Dr Schlaudecker reported grants from the US Centers for Disease Control and Prevention during the conduct of the study and grants from Pfizer and advisory committee service from Sanofi Pasteur outside the submitted work. Dr Laughon reported grants from the National Institutes of Health and the US Food and Drug Administration outside the submitted work. Dr Walter reported grants from Pfizer (investigator for clinical trial), Moderna (investigator for clinical trial), Sequiris (investigator for clinical trial), Najit Technologies (investigator for clinical trial), and Clinetic (investigator for clinical trial) and personal fees from Vaxcyte (advisory board), Pfizer (advisory board), Iliad Biotechnologies (consultant), and Shionogi (data safety monitoring board) outside the submitted work. No other disclosures were reported.
These two clinical trials are not valid for policy guidance. In addition, here also, the trial participation criteria and decisions for inclusion are not representative of the real world of global infant vaccination campaigns.
Clinical experience and research have long informed us that infant and child mortality in low-income countries is far more complex than the arguably irrelevant tunnel-vision view of specific pathogens and so-called immunization campaigns against the said specific pathogens (England, 1978; Hendrickse, 1975). Likewise, epidemiology informs us that factors other than vaccination overwhelmingly determine improvements in infant mortality (Ahmad et al., 2000; Armstrong et al., 1999; Black et al., 2003; Cutler and Miller, 2004; Cutler et al., 2006; Hendrickse, 1997; Humphries and Bystrianyk, 2015; Jones et al., 2003; Liu et al., 2016; McKinlay and McKinlay, 1977; Scrimshaw, 2003; Scrimshaw et al., 1968). These points should be recognized by all public health researchers, including those using theoretical models.
Comments of early informed skeptics are noteworthy.
In the words of tropical medicine researcher Hendrickse (1975):
… there is considerable danger that the benefits of measles vaccination will not measure up to expectations either in respect of reducing costs of treating the sick or in respect of reduction in childhood mortality. The reasons for this belief are:-
(1) Most estimates of measles mortality in developing countries have been extrapolated from hospital experience and such extrapolation is notoriously unreliable.
(2) All available evidence indicates that Protein Energy Malnutrition is one of the main determinants of measles morbidity and mortality in developing countries. Most deaths from measles occur in children whose weights fall below the 10th centile for age, and the disease is particularly lethal in children with kwashiorkor, an illness which has a high mortality rate in its own right.
(3) A very high proportion of those who die of measles succumb after the acute phase of the disease, in the so-called post-measles phase, from complicating infections such as bronchopneumonia and gastro-enteritis. …
It is pertinent to recall that 100 years ago measles was as serious a problem in Europe as it is in Africa today, yet the death rate from this disease and many other infectious diseases declined to negligible proportions with improvement in living standards long before vaccines became available.
Regarding the latter pivotal point of Hendrickse (1975), see: Armstrong et al. (1999), Humphries and Bystrianyk (2015) and McKinlay and McKinlay (1977).
In the published post-presentation discussion of the Hendrickse (1975) paper, the following points inter alia emerged:
Note that the dogma of measles as a primary cause of death in low-income countries is expertly put into doubt and is judged to be unlikely.
England (1978) summarized the situation this way: “Acute diarrheal disease and infections of the upper respiratory tract, whether presented or not, undoubtedly represent the most widespread causes of mortality and morbidity in poorer countries. Both are invariably clinical syndromes ‘.... that include a minority of known disease entities, a predominating bulk of undifferentiated, presumably infectious processes, and an indefinite number of non-infectious illnesses.’ (Scrimshaw et al., 1968)”
Both Hendrickse (1975) and England (1978) anchored some of their positions in the colossal work of Scrimshaw et al. (1968), which has been confirmed in the decades that followed (Scrimshaw, 2003). There is presently little doubt that immune dysfunction (via the gut microbiome) and susceptibility to varied (full spectrum) infections is overwhelmingly determined by nutritional status and deficiencies, especially in low-income countries and communities (Bailey et al., 2015; Gombart et al., 2020; Katoch, 2022; Katona and Katona-Apte, 2008; Keusch, 2003; Rodiguez et al., 2011; Scrimshaw, 2003; Scrimshaw et al., 1968). Likewise, similarly to any natural infection, even a mild immune response from vaccination is a challenge that can accelerate death in a malnourished infant or child, and Scrimshaw et al. (1968) reported such rarely documented cases.
Basically, in the absence of environmental toxicity, non-specific malnutrition (including of the mother) makes an infant or child highly vulnerable to death associated with a large array of possible infections ― infections that do not occur or are not fatal or debilitating in well-nourished individuals in healthy environments. Recognized global studies quantify this, thus showing that the vaccination programmes have relatively little potential to save lives (Black et al., 2003; Jones et al., 2003; Liu et al., 2016). This follows the conceptual framework proposed by Mosley and Chen (1984), which excludes dominance aggression, violence and addictions.
As such, immune dysfunction and infections are the main proximal causes of infant death in low-income countries. The corresponding risk of infant death depends on both fitness (primarily dependent on nutritional deficiencies) and exposure (primarily dependent on living and public-health conditions). Fitness is the dominant factor in circumstances of severe malnutrition, whereas exposure contributes significantly to infant mortality where strong environmental toxins and virulent pathogens and parasites are prevalent.
Here, the said exposure to strong environmental toxins and virulent pathogens and parasites is not exposure to the specific pathogens for which vaccines are typically developed and marketed. Rather, the strong environmental toxins are, for example, aflatoxin produced by fungi growing on staple foodstuffs in hot climates, which can be transferred by mother’s milk (Hendrickse, 1997); and the said virulent pathogens and parasites are, for example, waterborne parasitic protozoa of faecal origin (Baldursson and Karanis, 2011; Cutler and miller, 2004). Then, such strong exposures can significantly contribute to infant mortality, even with moderate prevalence of malnutrition or in the absence of malnutrition.
With sufficiently severe malnutrition, ambient exposures, including challenge by vaccination, will always be enough to cause large infant mortality, in the same way that prolonged droughts and high winds will always find sparks to start fires, whether from lightning or cooking fires or any other source. Likewise, history teaches us that it is difficult to have low mortality without a supply of water uncontaminated with protozoa and parasites from faecal matter.
In fact, frequency of exposure to virulent pathogens and parasites is overwhelmingly determined by sanitary conditions and access to non-contaminated water, historically (Cutler and Miller, 2004), and especially in low-income countries. Outbreaks of human diseases due to the waterborne parasitic protozoa (of faecal origin) continue to be common worldwide, and there is no systematic surveillance in the most affected low-income countries (Baldursson and Karanis, 2011). Resulting diarrhea is a leading cause of death in young children. Yet, access to non-contaminated water continues to be a major global problem (UN, 2019), while complex (cold chain, etc.), unproven (Section 4.1), constant universal and increasing vaccination programmes continue to be prioritized and imposed.
The same continuation and inaction is true of extreme poverty and so-called food insecurity crises (UN, 2023).
It is hypocritical and unconscionable for influential forces to coerce low-income countries to accept and implement universal infant vaccination programmes while impeding structural changes (i.e., development) that would eliminate chronic malnutrition, contaminated water, unsafe food storage, and urban slums (Centre for Applied Research, Norwegian School of Economics et al., 2015; Fernandez and Hendrikse, 2020).
Not only are high-priority public-health resources lacking but the vaccination campaigns necessarily divert structural and staff resources away from the provision of rudimentary health and emergency services (Hendrickse, 1975; Dietz and Cutts, 1997), including the list provided by Jones et al. (2003). Diplomatic authors have referred to “efficacy versus effectiveness” and “vertical versus horizontal” health programmes, while admitting that the provisions of vaccination programmes are “controversial” (Clemens et al., 1996; Dietz and Cutts, 1997; Mills, 1983). Mostly, however, the question has recently become in-effect taboo.
The hypothetical number of deaths (D0, in Equation 1) that would occur from the presumed pathogen in the absence of presumed-beneficial vaccination against the presumed pathogen does not rely on any determination or assumed value of the presumed vaccine efficacy (Ev, in Equation 1). Rather, D0 is a theoretical number of deaths that the modeller believes would have occurred (counterfactual) or will occur (forecast) from a presumed pathogen of choice, in the absence of any vaccination for the said presumed pathogen, all other factors being retained.
Therefore, D0 is a theoretical number of deaths caused by a chosen presumed pathogen (e.g., the measles virus) which would have been entirely averted if one had magically made the said chosen presumed pathogen perfectly benign (disappeared), in the population and time period of interest, all other factors acting the same. While this is an elegant (and apparently enticing) thought experiment, it is incompatible with how death actually occurs. In reality, the deaths of concern are always complex non-linear events that involve several interacting contributing factors that do not have additive effects. This means that the effect of a given agent or condition depends on the presence of other agents or conditions contributing to the death (or survival). Removing one agent (the chosen presumed pathogen) does not leave the effects of the other agents and conditions unchanged. For example, there is a large body of work on the interactions (both positive and negative) between the primary cause of death that is nutritional deficiencies and ambient infections, as amply discussed in Section 4.3.
So, strictly speaking, it is impossible to calculate D0, and its very definition is incompatible with biological reality.
If the modeller nonetheless decides to ignore this fundamental difficulty and insists on calculating D0, then they are left with equally impossible tasks such as:
Insisting on calculating D0 and on using it in providing policy guidance for national and subnational populations is an ideological exercise, not a scientific one.
As shown above in Section 3 and Figure 1, my analysis of global infant mortality rate compared to global vaccine coverage rollouts shows that there are approximately 100 million vaccine-rollout-associated infant deaths, 1974-2024 worldwide, not deaths averted by the vaccines.
My conclusion that there is a global excess infant mortality associated with the global vaccine coverage rollouts is independent of clinical trials of vaccine safety and efficacy (Ev), and is independent of estimates of counterfactual mortality (D0) that would have occurred if presumed-beneficial vaccination interventions had not been implemented.
Rather, my estimate of a vaccine-rollout-associated global excess infant mortality instead relies on the directly observed and model-independent changes in actual infant mortality rate (panel A, Figure 1) occurring synchronously with major vaccine coverage rollouts (Figure 1). The observed infant mortality rate increases (i.e., positive changes in slope, or decelerated declines of infant mortality) at times of increasing vaccine coverage per year: in a first generation of vaccine rollouts, 1980-1990, and in a second generation of vaccine rollouts, 1990-2015 (Figure 1). Here, the deceleration in the decline of infant mortality is greater for the said second generation of vaccine rollouts, starting with hepatitis B and PCV (pneumococcal conjugate vaccine) vaccines in approximately 1992 (Figure 1). The important deceleration of decline in infant mortality is also apparent for low-income countries in the extensive quantitative work of Ahmad et al. (2000), regarding aged < 5 years child mortality in the large regions of the world. The said deceleration was not explained, and is puzzling given the large potential for improvement, yet it occurs in the years of most vaccine coverage by the most vaccines.
The evident temporal correlation between deceleration of decline in infant mortality and increasing vaccine coverage with more vaccines (Figure 1) is an immediate epidemiological observation disregarded by all theoretical modelling researchers calculating presumed vaccine benefits on global infant mortality.
My necessarily positive quantitative estimate of approximately 100 million global excess infant deaths associated with the global vaccine coverage rollouts is obtained from the apparent gap between expected infant mortality rate linearly inferred from periods prior to the vaccine rollouts (green and purple line extrapolation scenarios in panel A, Figure 1) and the actual infant mortality rate (with implementation of the vaccine rollouts) (black solid line, panel A, Figure 1). The said gap is approximately 100 million infant deaths, 1974-2024, worldwide.
Here, my said “expected infant mortality rate linearly inferred from the period prior to the vaccine rollouts” is a counterfactual of infant mortality if the vaccines had not been implemented. Unlike the counterfactuals in the modelling papers of deaths averted by vaccination (Ls, Equation 1, Section 1), my counterfactual is based entirely on estimating the trend of continuously decreasing infant mortality from improving living conditions in the absence of vaccination. It does not rely on:
The linear extrapolation scenarios that I consider (green and purple lines in panel A of Figure 1) are the simplest model-independent approach. Any resulting estimate needs to be adjusted for the saturating benefits of improving living conditions (actual infant mortality cannot be zero or negative).
An important caveat regarding my counterfactual using linear extrapolation is the following. The 1990s saw a spectacular increase in aggressive so-called globalization (economic predation), following the early 1990s dissolution of the Soviet Union (USSR), continuing until today. This was accompanied by largescale unsafe industrial practices such as an accelerated use of the herbicide glyphosate and increases in vaccination programmes of all types (Rancourt, 2019). Health and mortality impacts in low-income countries from this hyper-globalization could have been varied and significant. See: Centre for Applied Research, Norwegian School of Economics et al. (2015); Rancourt (2019). Similarly, there were large global structural financial adjustments and socioeconomic consequences in the 1980s following China’s joining of the World Bank in 1980 and so-called reform and opening-up (Committee et al., 2018: “The early 1980s marked the emergence of what now may be considered the modern era of homelessness.”). More on-point, poverty in Sub-Saharan Africa and inequity in Africa increased significantly in the 1980s (Sala-i-Martin and Pinkovskiy, 2010, their figures 5 to 10 and 12 to 14).
It has been inconvenient for the vaccine industry that several repeated observational studies have shown a many-fold (up to 5-fold) increase in infant mortality with the introduction and administration of the diphtheria-tetanus-pertussis (DTP) vaccine in low-income countries (Aaby et al., 2012, 2016, 2018; Mogensen et al., 2017).
This led to what can be called an organized attempted cover up by the WHO (see Aaby et al., 2016; and see Aaby et al., 2018 and Mogensen et al., 2017). It is not unusual for the WHO to work to systemically avoid acknowledging significant evidence of vaccine harm (Puliyel and Naik, 2018).
The said observational studies typically monitored all-cause deaths from first regular clinic visit for typically up to 3 years of age in both vaccinated and unvaccinated children within clinic catchment regions in a low-income country. The selection bias for vaccination is expected to be that the frailest are less vaccinated. Therefore, the expected result from this bias is that the vaccinated would have lower all-cause mortality but the opposite occurs, despite any presumed life-saving benefit from the DTP vaccination.
It is difficult not to conclude that DTP vaccination campaigns caused large increases in infant mortality in low-income countries, as indicated in Figure 1, to say nothing of unknown deleterious interactions between different vaccines.
Contrary to notions of safety and efficacy of infant and childhood vaccinations, several authors having no industry interests report:
Main limitations on my estimate of approximately 100 million vaccine-programme-associated deaths, 1974-2024 worldwide (Section 5.1), are as follows: